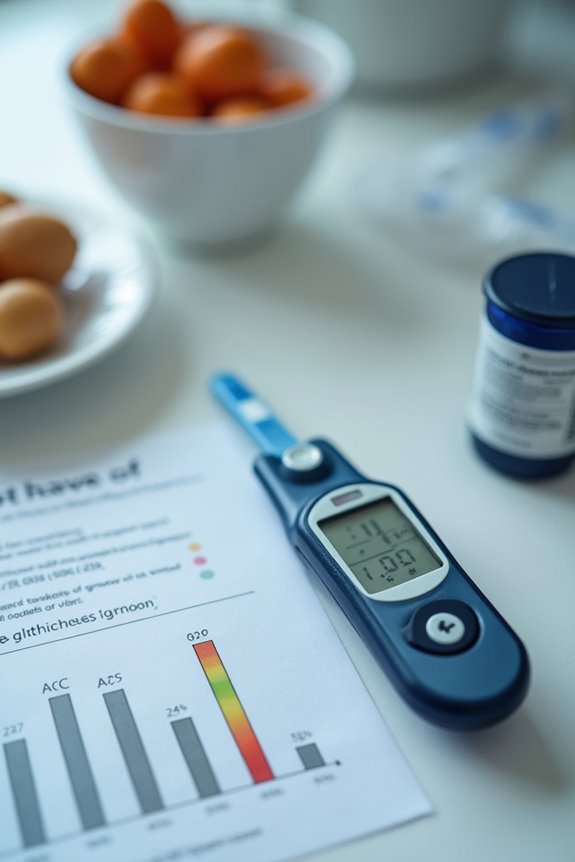
The A1C test measures average blood glucose levels over 2-3 months, specifically the percentage of glycated hemoglobin (HbA1c). Normal values are below 5.7%, with prediabetes ranging from 5.7% to 6.4%, and diabetes at 6.5% or higher. Testing frequency varies: those with prediabetes should be tested annually, while insulin users may require more frequent evaluations. Maintaining an A1C under 7% is essential for health. Further details on managing A1C levels and understanding blood sugar can enhance diabetes management.
Key Takeaways
- The A1C test measures average blood glucose levels over 2-3 months, reported as a percentage of glycated hemoglobin.
- Normal A1C levels are below 5.7%, while prediabetes and diabetes are indicated by levels of 5.7%-6.4% and 6.5% or higher, respectively.
- A1C does not reflect daily glucose fluctuations and can be affected by conditions like anemia or kidney disease.
- Regular testing is vital; stable patients should test twice a year, while those with prediabetes should test annually.
- Lifestyle changes, including diet and exercise, play a significant role in managing blood sugar and lowering A1C levels.
What Is the A1C Test?
The A1C test is an essential tool in the management and diagnosis of diabetes. It provides an average of blood glucose levels over the previous two to three months by measuring the percentage of glycated hemoglobin. This test is critical for diagnosing type 2 diabetes and prediabetes, as well as monitoring the effectiveness of diabetes management strategies.
Key points about the A1C test include:
- Normal A1C levels are below 5.7%.
- Levels between 5.7% and 6.4% indicate prediabetes.
- Levels of 6.5% or higher suggest diabetes.
Despite common A1C misconceptions, this technology offers a reliable snapshot of long-term glycemic control, unaffected by short-term fluctuations. Understanding the A1C test is crucial for effective diabetes care.
How the A1C Test Works
Understanding how the A1C test operates is essential for both healthcare providers and patients managing diabetes.
A1C Mechanisms
The A1C test quantifies the percentage of glycated hemoglobin (HbA1c) in the blood, formed through the glycation process. Glucose binds to hemoglobin in red blood cells, creating stable glycated hemoglobin over an average lifespan of three months.
Test Procedure
A blood sample is drawn, often from a vein, without the need for fasting.
Laboratory Analysis
The sample undergoes analysis, yielding a percentage that reflects average blood glucose levels over 2-3 months. Elevated percentages indicate poorer glucose control, while lower percentages suggest better management and absence of diabetes risk factors.
Ultimately, the A1C test provides a long-term view of glucose control.
Interpreting A1C Results

Interpreting A1C results is essential for evaluating an individual’s glucose management and diabetes risk. The A1C test measures average blood glucose over the past three months, reported as a percentage.
A1C Categories:
- Normal: Below 5.7%
- Prediabetes: 5.7% to 6.4%
- Diabetes: 6.5% or above on two separate tests
Clinical Significance:
- A1C below 5.7% indicates normal blood sugar control.
- A1C between 5.7% and 6.4% signals increased diabetes risk.
- A1C 6.5% or above confirms diabetes if repeatable.
Target Goals:
– For most adults with diabetes, target A1C is less than 7%.
A1C interpretation is integral for effective risk assessment and personalized diabetes management.
Relationship Between A1C and Blood Sugar Levels

Examining the relationship between A1C and blood sugar levels reveals critical insights into diabetes management.
- A1C Significance: A1C strongly correlates with average blood glucose levels in diabetic patients, reflecting long-term glucose control over the past 2 to 3 months. This correlation is particularly strong, with studies indicating an r² of approximately 0.87 to 0.96.
- Blood Sugar Variability: In contrast, blood sugar measurements provide immediate glucose levels and can fluctuate due to meals or activity. Single glucose readings correlate less reliably with A1C, emphasizing the need for averaged values.
- Measurement Differences: A1C is expressed as a percentage, while blood glucose is measured in mg/dL. Understanding these different units aids in interpreting their relationship effectively.
Importance of A1C in Diabetes Management

The significance of A1C in diabetes management cannot be overstated, as it serves as an essential indicator of long-term glycemic control.
- A1C reflects average blood sugar levels over the past 2 to 3 months, providing a reliable measure of chronic blood glucose control.
- Regular A1C monitoring allows healthcare providers to assess treatment effectiveness and make necessary adjustments.
- The American Diabetes Association recommends testing at least twice yearly, with more frequent assessments for those not meeting blood sugar goals.
- Maintaining A1C levels near or below 7% is linked to improved health outcomes and reduced risks of complications, including microvascular and macrovascular diseases.
- Individualized A1C targets enhance patient care, balancing the risks of tight control against potential benefits.
Limitations of the A1C Test
How reliable is the A1C test as a measure of diabetes management? While the A1C test is a valuable tool, it has notable limitations that can affect its accuracy.
A1C Inaccuracies****
– Conditions like anemia and chronic kidney disease can lead to falsely elevated or lowered results.
Diagnostic Limitations
– A1C may miss early diabetes cases detectable by oral glucose tolerance tests.
Glycemic Variability
– It does not reflect daily glucose fluctuations or acute spikes, which can be critical for management.
External Factors
– Variability in laboratory methods and individual differences in glycation can skew results.
Frequency of A1C Testing
Determining the appropriate frequency of A1C testing is essential for effective diabetes management, as it helps healthcare providers monitor patient progress and treatment efficacy.
Recommended Testing Frequency:
- Prediabetes: Annual testing.
- Stable Patients (no insulin): Twice a year if blood sugar levels are within target.
- Unstable Patients or Medication Changes: Every three months.
- Insulin Users: More frequent testing may be necessary.
Adjustment Factors:
- Testing intervals can be modified based on individual treatment plans and patient stability.
- Less frequent testing may be justified if glycemic targets are consistently met, potentially extending intervals to six months or longer.
Healthcare providers tailor testing frequency to each patient’s unique needs, ensuring ideal diabetes management and control.
A1C Targets for Diabetes Management
What A1C targets are most effective for diabetes management? The American Diabetes Association (ADA) recommends several A1C targets based on individual patient factors:
- <7% (53 mmol/mol) for many nonpregnant adults.
- <6.5% (48 mmol/mol) for selected patients without significant hypoglycemia risk.
- <8% (64 mmol/mol) for individuals with severe hypoglycemia history or advanced complications.
Individualized targets are essential to balance glycemic control benefits against risks like hypoglycemia. Approximately 31% of U.S. adults with diabetes achieve the <7% target, while 69% may require less stringent goals. A1C variability impact highlights the importance of tailoring management strategies to each patient’s unique circumstances, ensuring safety and effective long-term outcomes. Individualization fosters better health and aligns treatment with patient preferences and needs.
Comparing A1C With Other Blood Sugar Tests
A1C testing plays a significant role in diabetes management, but it is important to understand how it compares with other blood sugar tests.
- A1C Overview: Measures average blood glucose over 2 to 3 months; expressed as a percentage or estimated average glucose (eAG).
- Blood Glucose Tests: Provide immediate snapshots of glucose levels; include fingerstick and continuous glucose monitoring.
- A1C Accuracy: Less influenced by daily fluctuations, making it suitable for long-term monitoring.
- Blood Glucose Variability: Captures short-term changes, essential for daily management and detecting hypoglycemia or hyperglycemia.
- Complementary Roles: A1C is used for diagnosing diabetes, while blood glucose tests assess acute changes. Both tests are necessary for thorough diabetes management, addressing different aspects of glucose control.
Tips for Maintaining Healthy A1C Levels
Maintaining healthy A1C levels is essential for effective diabetes management, as elevated levels can lead to serious health complications. Individuals can achieve ideal results through several key strategies:
- Lifestyle Changes: Implement dietary modifications, focusing on moderating carbohydrate intake and practicing portion control.
- Exercise Routines: Regular physical activity not only lowers A1C levels but also enhances overall health.
- Hydration Strategies: Staying adequately hydrated supports stable blood sugar levels.
- Medication Adherence: Consistent use of prescribed medications guarantees effective blood sugar management.
- Stress Reduction: Employing techniques for stress management can prevent blood sugar spikes.
Incorporating healthy lifestyle changes can significantly improve your blood sugar levels and overall well-being.
These elements work collaboratively to help individuals maintain A1C levels below 7%, promoting better health outcomes and reducing the risk of complications.
Frequently Asked Questions
Can Diet Affect My A1C Levels Significantly?
A low-fat vegan diet can reduce A1C by 0.8%, illustrating the profound impact of dietary changes. Through glucose monitoring, individuals can witness their journey toward improved health, fostering a sense of community and shared success.
How Quickly Can A1C Levels Change With Treatment?
A1C fluctuations typically require 2 to 3 months to reflect treatment adherence changes. Consistent medication adjustments, lifestyle modifications, and monitoring can lead to meaningful reductions, fostering a sense of community among those managing diabetes together.
What Medications Can Influence A1C Results?
Medications considerably influence A1C results, impacting diabetes management. Insulin therapy and oral medications can alter blood sugar levels. Medication adherence is essential, as variations in treatment can affect overall glycemic control and A1C measurements.
Is There a Specific Time of Day for Testing A1C?
As uncertainty looms over ideal testing times, many wonder about morning versus evening testing. While mornings often yield stable results, evening tests can also be acceptable, emphasizing the importance of consistent conditions for accurate assessments.
Can Stress Impact My A1C Reading?
Stress can greatly impact A1C readings, as elevated cortisol levels from stress may disrupt glucose metabolism. Effective stress management strategies are essential for individuals seeking to maintain balanced A1C levels and foster a supportive community.




