Understanding dosage for children’s medicines is essential for safety and efficacy. Weight-based dosing minimizes errors, as 3.7% of pediatric medication errors result from inaccurate weight data. Body Surface Area (BSA) scaling offers a precise approach, correlating with physiological needs. Dosing complexities often lead to miscalculations, compounded by unit conversion mistakes. Safe administration practices include using pediatric oral syringes for accuracy and verifying medication against doctor orders. Additional insights can enhance caregiver understanding and reduce risks associated with medication administration.
Key Takeaways
- Weight-based dosing is crucial for accurate medication administration in children, preventing underdosing or overdosing.
- Body Surface Area (BSA) scaling offers a more precise dosing method tailored to a child’s physiological needs.
- Common errors in pediatric dosing often stem from weight measurement mistakes and confusion over multiple formulations.
- Caregivers should always read medication labels carefully and use appropriate dosing tools for accuracy.
- Healthcare providers must communicate effectively with caregivers to ensure understanding of dosing instructions and safety measures.
Importance of Weight-Based Dosing
Weight-based dosing is crucial in pediatric medicine, as it guarantees that medication administration is tailored to the individual characteristics of children. Accurate weight measurement is essential at each encounter, as it helps to prevent underdosing or overdosing, thereby minimizing the risk of adverse drug events.
Key statistics include:
- Approximately 3.7% of pediatric medication errors stem from missing or inaccurate weight data.
- Electronic prescribing systems lacking weight input greatly increase medication errors.
Weight-based dosing reduces dosing variability, promoting more predictable drug effects in children compared to fixed dosing methods. This tailored approach enhances both safety and efficacy, ensuring that children receive appropriate therapeutic interventions based on their unique body weight.
Body Surface Area (BSA) Scaling Explained
Body surface area (BSA) scaling is a crucial component in pediatric medicine, ensuring that medication dosages are precisely tailored to a child’s physiological needs. BSA is calculated using methods such as the West nomogram or the formula ( A = sqrt{frac{W (kg) times H (cm)}{3600}} ).
BSA Dosing Advantages:
- Provides a more accurate representation of body size than weight alone.
- Correlates with physiological parameters like cardiac output and renal function.
- Reduces dosing variability among children of different sizes.
This method is particularly essential for medications with narrow therapeutic windows, minimizing the risk of toxicity or underdosing. BSA dosing facilitates safer, more effective treatment while accommodating the unique metabolic capacities of pediatric patients.
Common Errors in Pediatric Dosing

Medication errors in pediatrics represent a significant challenge in healthcare, particularly due to the unique physiological characteristics and developmental stages of children. Common errors in pediatric dosing often stem from several factors:
- Dosing Complexities: Individualized dosing calculations based on weight can lead to frequent inaccuracies.
- Weight Measurement Mistakes: Using incorrect units, such as kilograms instead of pounds, contributes to significant errors.
- Pediatric Formulations: The availability of multiple formulations can create confusion among healthcare providers.
- Communication Issues: Misunderstandings during verbal prescriptions can lead to critical dosing mistakes.
These errors not only pose risks of overdosing or underdosing but also highlight the need for improved systems and protocols in pediatric medicine to enhance safety and efficacy in medication administration.
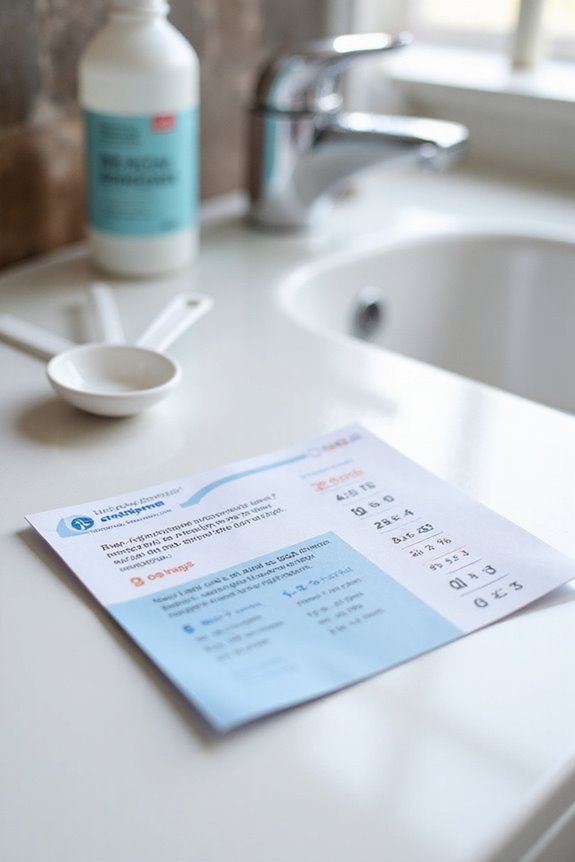
Safe Practices for Administering Children’s Medications
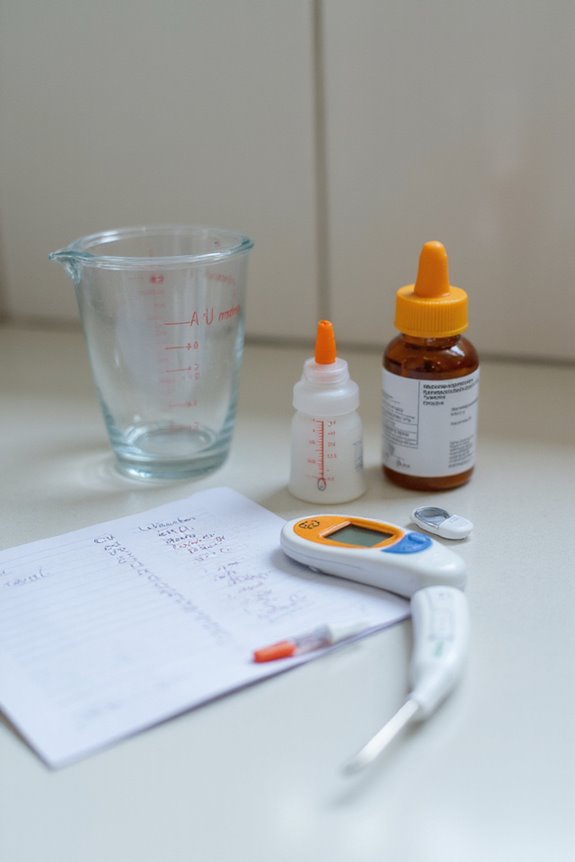
Administering children’s medications requires meticulous attention to detail to guarantee safety and effectiveness. Implementing best practices is essential for medication safety.
Verification Steps:
- Confirm the child’s name on the prescription.
- Verify the medicine aligns with the doctor’s orders.
- Review all labels and inserts for critical information.
Measurement Techniques:
- Utilize pediatric oral syringes for accurate dosing.
- Avoid household utensils for measurement.
Storage Recommendations:
- Store medications out of children’s reach and in original containers.
- Use child-proof caps, recognizing their limitations.
Supervision Protocols:
- Administer medications in well-lit areas.
- Stay with the child until ingestion is complete.
Emergency Preparedness:
– Know each medication’s purpose and contact emergency services if needed.
Dosage Recommendations for Common Medications

When determining appropriate dosages for common pediatric medications, it is vital to evaluate weight, age, and specific medical conditions.
Amoxicillin
- Children > 3 months to 40 kg: 20-40 mg/kg/day in divided doses every 8 hours.
- Endocarditis prophylaxis: 50 mg/kg (max 2 g) before procedures.
Ibuprofen
- Not recommended for children under 6 months.
- Dosing frequency: Every 6 hours as needed.
Diphenhydramine HCl (Benadryl)
– Children under 1 year: Use only if advised by a pediatrician.
Acetaminophen
– May be given every 4 hours, max five doses in 24 hours.
These guidelines, along with antibiotic guidelines for pediatric analgesics, guarantee safe medication administration.
Challenges in Current Pediatric Dosing Guidelines
Current pediatric dosing guidelines are often hindered by various challenges that complicate the safe and effective administration of medications to children.
- Pediatric Trial Limitations: Recruitment issues arise due to parental reluctance, limiting data on safety and efficacy.
- Ethical Concerns: These concerns restrict thorough research across pediatric age ranges, making precise dosing difficult.
- Physiological Variability: Differences in drug absorption and metabolism among various developmental stages complicate uniform dosing recommendations.
- Formulation Issues: Approximately 15% to 37% of pediatric medications require manipulation, leading to inaccuracies and potential safety risks.
- Regulatory Barriers: Operational hurdles deter investment in pediatric medicine development, resulting in a lack of age-appropriate formulations and extensive labeling.
These factors collectively hinder the establishment of reliable dosing guidelines.
Consequences of Inaccurate Dosing
Inaccurate dosing of pediatric medications can lead to considerable consequences that compromise patient safety and treatment efficacy. The implications of dosing errors include:
- Increased Risk of Adverse Reactions: Children are more vulnerable due to their developing physiology, leading to potentially life-threatening reactions.
- Higher Frequency of Errors: Pediatric errors occur three times more often compared to adults, underscoring the urgency of addressing this issue.
- Impact on Treatment Efficacy: Both overdoses and insufficient doses can considerably reduce treatment effectiveness.
- Economic Burden: Medication errors strain healthcare systems through increased hospitalizations and resource utilization.
Implementing rigorous safety measures is essential to mitigate these risks and enhance the overall safety of pediatric medication administration.
Strategies to Improve Dosing Accuracy
Effective strategies to improve dosing accuracy in pediatric medicine are critical for enhancing patient safety and treatment outcomes. Key approaches include:
- Standardization: Weight-based dosing simplifies calculations, minimizing errors and facilitating accurate dose projections through established methods like the Salisbury rule.
- Utilization of Pediatric Tools: Devices such as the Broselow Pediatric Emergency Tape and standardized formularies help clinicians estimate dosages quickly and reduce confusion.
- Digital Dosing Calculators: Integration of automated systems in pre-hospital and hospital protocols supports cognitive offloading, ensuring precise dosing in emergencies.
- Training and Protocol Alignment: Ongoing education about pediatric-specific guidelines is essential to address clinician discomfort and promote adherence to national recommendations.
These strategies collectively enhance the accuracy of medication dosing in pediatric care, ensuring safer treatment for children.
Educating Caregivers on Medication Measurement
Educating caregivers on medication measurement is an essential component of pediatric healthcare, building upon strategies for improving dosing accuracy. Proper use of medication tools and dosing devices is critical to guarantee safe administration.
Key Considerations:
- Accurate Measurement: Use oral syringes, dosing cups, or spoons specifically designed for medications to avoid inaccuracies.
- Volume Clarity: Always measure dosages in milligrams (mg) rather than milliliters (mL) to account for varying concentrations.
- Body Weight Conversion: Calculate dosages based on body weight, guaranteeing correct conversion from pounds to kilograms.
- Reading Labels: Caregivers should carefully read medication labels for dosing instructions and age restrictions.
The Role of Healthcare Providers in Pediatric Dosing
The role of healthcare providers in pediatric dosing is essential, as they must navigate the complexities of medication administration tailored to children’s unique physiological characteristics. Effective provider communication is critical, ensuring caregivers understand dosing instructions through advanced counseling techniques, such as teachback and dose demonstration.
- Pediatric training equips providers with the skills to calculate doses accurately based on height and weight.
- Regular training on these strategies is necessary to integrate best practices into routine care.
- National organizations advocate for policy measures to enhance pediatric readiness in emergency settings, addressing common dosing challenges.
Frequently Asked Questions
How Can I Track My Child’s Weight Accurately for Dosing?
To track a child’s weight accurately, regular weight monitoring is essential. Recording measurements on growth charts helps visualize progress, ensuring a sense of belonging in the journey of healthy growth and development for the child.
Are Natural Remedies Safe for Children Alongside Prescribed Medications?
Despite the appeal of natural remedies, their safety alongside prescribed medications remains uncertain. Potential medication interactions necessitate careful consideration, emphasizing the importance of consulting healthcare professionals to guarantee children’s safety and well-being in treatment choices.
What Should I Do if My Child Misses a Dose?
If a dose is missed, it is advisable to administer it as soon as possible unless close to the next scheduled dose. Consistency in maintaining the medication schedule is essential for effective treatment.
Can I Use Adult Medications for My Child in Emergencies?
In emergency situations, using adult medications for children poses significant risks. Precautions are vital, as even minor doses can be harmful. Always consult a healthcare professional to guarantee safety and appropriate treatment for pediatric needs.
How Often Should I Consult a Doctor About My Child’s Medication Needs?
In a world where health is paramount, consulting a doctor frequently for medication reviews guarantees children’s well-being. Following a physician’s advice fosters trust, while proactive engagement allows for timely adjustments and ideal care for every child’s unique needs.





